Cancer Survivorship and Chronic Disease
Image provided by Oncology Nurse Advisor.
Overview
“In my internal medicine training here at UCSF, I was struck by how much of my hospitalized patients’ disability could have been prevented,” says Dr. Sarkar. This observation led to our focus on empowering patients and health care teams to better manage chronic conditions. Supporting patients with chronic diseases in between visits is critical to improving health outcomes.
According to the the CDC, chronic diseases are responsible for 7 in 10 deaths each year, and treating patients with chronic diseases accounts for much of our nation’s health care costs. Cancer, one of the most prominent chronic diseases, afflicts more than 1.75 million people per year in the United States, and more than 16.9 million people in the U.S. are cancer survivors. Diabetes, a chronic disease that affects the pancreas and the body’s glucose levels, afflicts more than 37 million people in the U.S. with approximately 1.4 million new cases each year. Hypertension, a precursor to heart disease and one of the most prominent chronic diseases in the U.S., afflicts approximately 116 million people or 47% of the U.S. population. Other common chronic diseases include lung disease, kidney disease, arthritis, and Alzheimer’s disease, all of which are often exacerbated by socioeconomic disparities. Our lab is committed to eliminating barriers and improving the outcomes of all patients living with chronic diseases.
Current Projects
CRUISE Study
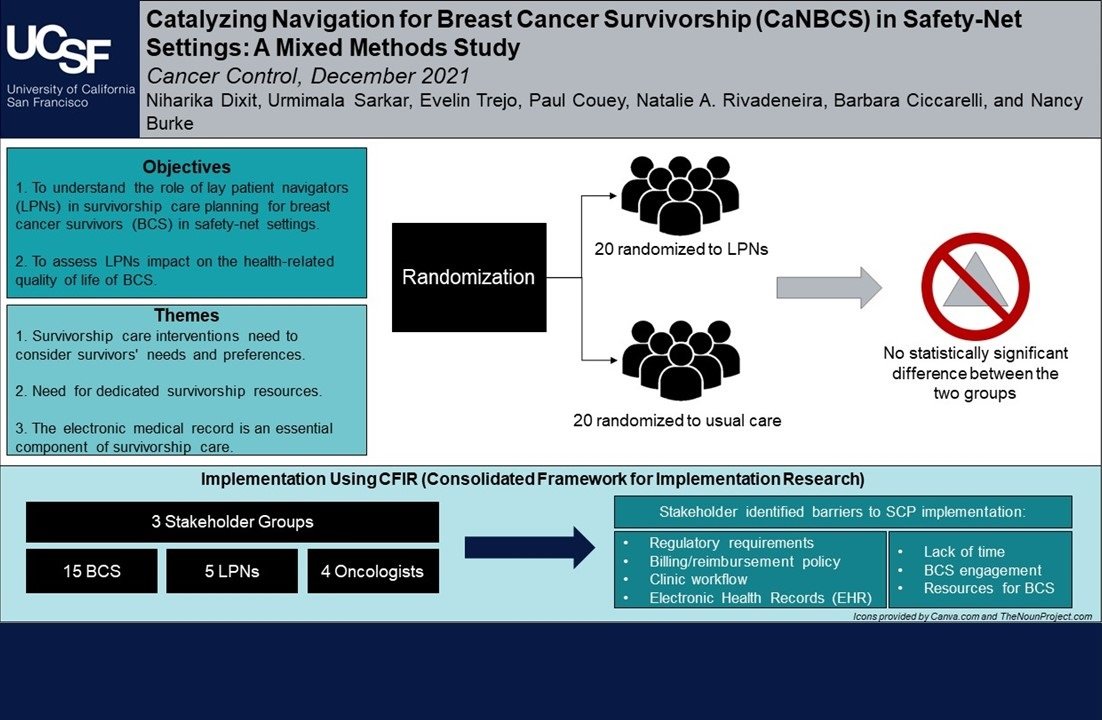
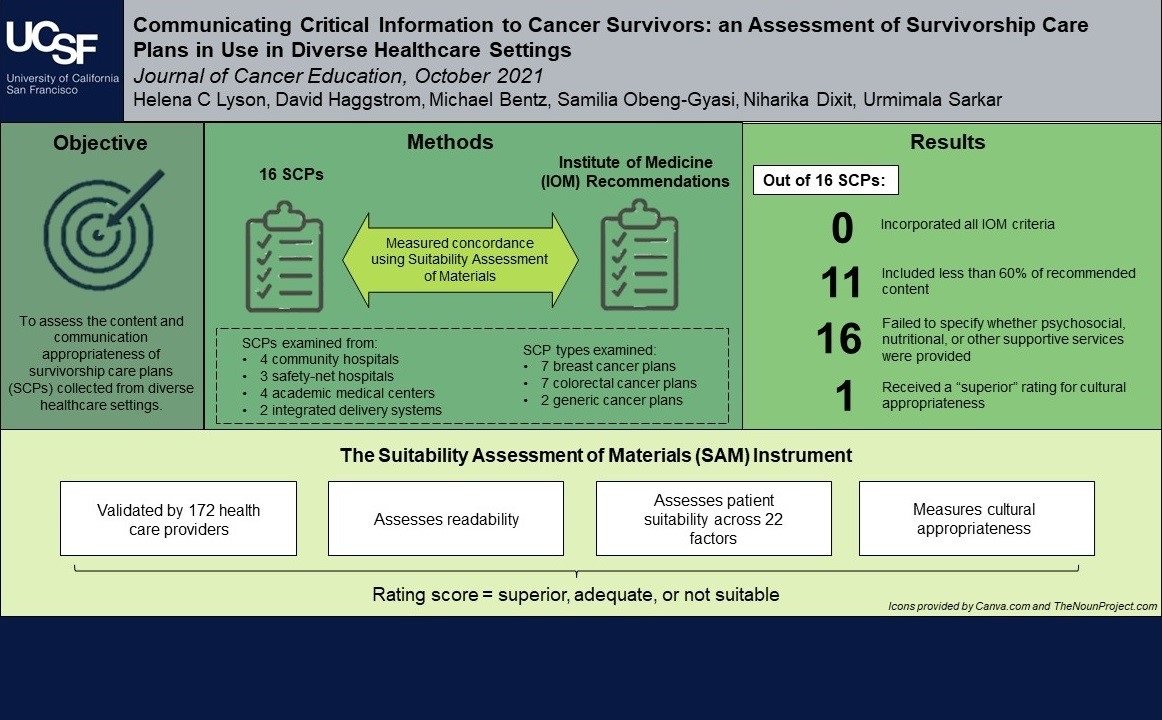
The goal of the ongoing Cancer Registry for Understanding and Improving Survivorship Experiences (CRUISE) study is to learn more about patient experiences following cancer treatment and to explore the information health care providers give patients during and after cancer treatment. To respond to the growing population of cancer survivors, providers and organizations such as the American College of Surgeons have developed guidelines for survivorship care plans (SCPs).
An analysis of 16 SCPs collected from a wide range of health care settings revealed that SCPs often fail to incorporate criteria recommended by the Institute of Medicine, and that significant variation exists among the structure and content of these plans. The delivery and content of SCPs for underserved populations has not been well-studied. Our sample includes English-, Spanish-, and Cantonese-speaking patients across the Greater Bay Area, as well as clinicians, staff, and administrators across a range of health care settings, including the medical safety-net. CRUISE takes a comprehensive, multilevel approach to identify barriers and facilitators to effective implementation of SCPs in real-world settings serving diverse patients.
IMPACTT
The IMProving Adherence to Colonoscopy through Teams and Technology (IMPACTT) study aims to improve colorectal cancer (CRC) screening among vulnerable populations. CRC is the second leading cause of cancer death in the United States. Despite the effectiveness of CRC screening, it is underused, and late-stage CRC and CRC-based mortality remain disproportionately high in racial/ethnic minority populations and in safety-net health systems. The IMPACTT study uses a multilevel approach to support and increase the completion of a diagnostic colonoscopy following an abnormal fecal immunochemical test (FIT) by patients in the San Francisco Health Network.
Thanks to The National Cancer Institute (NCI) for funding the CRUISE study (5R01 CA241128-04)
Selected Completed Cancer Survivorship Projects:

Cancer Survivorship and Chronic Disease Presentations:
Dr. Sarkar at the nAM: Health literacy and Communication Strategies in Oncology Conference in 2019
Health literacy is defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions. To address the needs of patients and families with low health literacy and improve health outcomes, we must develop literacy appropriate patient-facing communication across the care continuum.
Dr. Sarkar Discusses Patient-Clinician Communication & Strategies for Improving Equity in Diagnosis
Timely diagnosis, particularly for cardiovascular events, is critical for positive patient outcomes. Within-visit communication is complex and features various barriers including language access and health literacy. To improve equity in the diagnostic process, providers must embrace communication interventions such as providing patients with literacy-appropriate information.



